Bacteriophages and antibiotics
Mycobacterium abscessus, a relative of the bacteria that cause tuberculosis and leprosy, is responsible for particularly severe damage to human lungs and can be resistant to many standard antibiotics, making infections extremely challenging to treat. Researchers from the Université de Montpellier, France, and the University of Pittsburgh, have published a study (“Mycobacteriophage-antibiotic therapy promotes enhanced clearance of drug-resistant Mycobacterium abscessus”) in Disease Models & Mechanisms that describes the antibacterial effects of treating infections caused by the antibiotic-resistant bacteria M. abscessus with a bacteriophage and an antibiotic.
“Infection by multidrug-resistant Mycobacterium abscessus is increasingly prevalent in cystic fibrosis (CF) patients, leaving clinicians with few therapeutic options. A compassionate study showed the clinical improvement of a CF patient with a disseminated M. abscessus (GD01) infection, following injection of a phage cocktail, including phage Muddy. Broadening the use of phage therapy in patients as a potential antibacterial alternative necessitates the development of biological models to improve the reliability and successful prediction of phage therapy in the clinic,” write the investigators.
“Herein, we demonstrate that Muddy very efficiently lyses GD01 in vitro, an effect substantially increased with standard drugs. Remarkably, this cooperative activity was retained in an M. abscessus model of infection in CFTR-depleted zebrafish, associated with a striking increase in larval survival and reduction in pathological signs. The activity of Muddy was lost in macrophage-ablated larvae, suggesting that successful phage therapy relies on functional innate immunity.
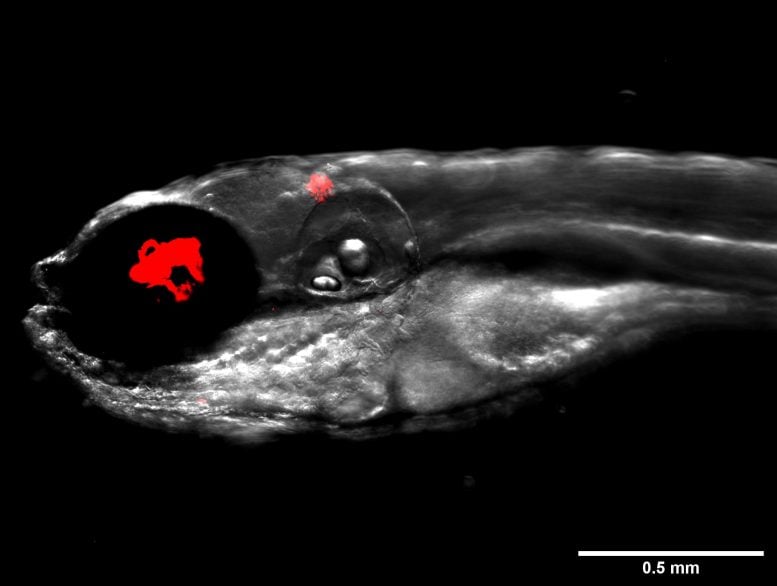
“CFTR-depleted zebrafish represent a practical model to rapidly assess phage treatment efficacy against M. abscessus isolates, allowing the identification of drug combinations accompanying phage therapy and treatment prediction in patients.”
Previously, the Pittsburgh team had identified one bacteriophage out of 10,000, known as “Muddy,” that efficiently kills bacteria in a petri dish and could be a candidate for treating these infections in humans. However, the team wanted to find an alternative to testing their new therapy in patients.
Source:
Johansen, M.D., et al. (2021) Mycobacteriophage–antibiotic therapy promotes enhanced clearance of drug-resistant Mycobacterium abscessus. Disease Models & Mechanisms. doi.org/10.1242/dmm.049159.


 Bacteriophage mediated control of necrotic enteritis caused by C. perfringens in broiler chickens
Bacteriophage mediated control of necrotic enteritis caused by C. perfringens in broiler chickens
